As I mentioned in a recent post, we have a process for instituting a STEMI alert to, in consultation with an ED doctor, activate the cath lab prehospitally based on clinical assessment and a 12-Lead ECG. The coordinator at the hospital that I transport most of my patients to told me so far EMS is batting 1000 when it comes to accurately calling STEMIs, but he did add the reason for that is EMS has been very conservative in calling for the cath lab. In other words, only the obvious STEMIs are getting called in. I can understand that as I am guilty of it myself. If I have an no-brainer, I don’t hesitate to call in, but I don’t want to call in a false alarm. The coordinator said he would like to see people being more aggressive, calling in to consult with the MD even in marginal cases. If the MD isn’t convinced, he can always delay calling until arrival at the hospital. The coordinator did say when EMS activated the cath lab, it is cutting door to balloon time in half.
I had this call the other day:
Chest pain at a local factory that employs a lot of temporary help, and where we are often called for get-out-of-workitsis. We find a muscular 40-year-old male with some serious Biggie Smalls gold bling around his neck. He is lying on the ground rolling around holding his chest. We wheel the stretcher over to him, and I, unimpressed, say, “Get on the stretcher,” which he does, although he continues to grimace quite excessively. There is a bit of coworker crowd there, so I say to my partner, let’s just get him out into the ambulance. I prefer working people in the ambulance. There is privacy. I have everything I need there, and if anything turns bad, we are already on our way to the hospital. Also, actors tend to cease their dramatics once they are in the ambulance, out of sight of their audience.
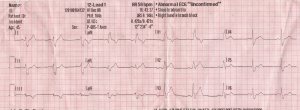
In the ambulance, I have him take off his shirt, which reveals a thick scar across his abdomen. He tells me got stabbed many years ago. His only current history is HTN, although he admits to a family cardiac history. He is quite muscular but denies any recent muscle strain. He was opening boxes at work when the pain started, but noting so strenuous to cause a muscle tear. The pain is substernal, squeezing and not affected by movement. While I take his vitals, which are quite good, my partner puts him on the monitor. The initial three lead looks a little funky. And then he comes the full 12-lead:
Okay so he has a right bundle branch block. I have to admit I have rarely seen a right bundle branch in a 45-year-old, and there is what I would call an atypical pattern in V2 and V3. It looks like an ST elevation coming off the bundle. Odd. I know a Left bundle branch block can obscure an MI, but I am not so sure about a right bundle. Still, it is enough for me to take a little more seriously than if he was in a perfect sinus.
I give him 02 by cannula, pop in a line, give the ASA and nitros (one every 5 minutes) which provide no relief. When I patch to the hospital — I do not call a STEMI alert, but I say something along the lines of “the patient has a right bundle branch block, but it is sort of funky troubling looking. No idea what his norm is.”
I do a bunch of serial ECGs and they are all the same. I should take some relief in that, but the last one I do, has something else troubling. The computer has decided to call the strip an “ACUTE MI SUSPECTED” even though it looks exactly like the other 12-leads.
At the hospital, I tell the nurse I am troubled and we both approach a doctor and show him the strip. I preface, by saying I know it is a right bundle, but it doesn’t look like a normal one. He is not certain what to make of it, so he walks over to the patient and starts questioning him, and agrees he needs the full cardiac workup. They draw labs, and hook him up to some heparin and nitro.
***
A week later I get the followup. About an hour after I left the ED, after consulting with cardiology, they take him up to the cath lab, where it is discovered he has a 90% lesion in the left anterior descending artery. For some reason they can’t cath him properly, so he ends up getting cardiac bypass.
Interesting call.
Here’s a final closer look at V1-V3
***
Some tidbits I learned about RBBB.
It is in fact very rare in men under 50 ( less than .7 percent of the population.)
RBBB
Gennerally speaking an RBBB does not obscure a STEMI like a LBBB can.
***
In researching other systems STEMI alerts, I discovered in Massachusetts there are some hospitals that have a dual STEMI alert. The medic can call in and say “I have a definite STEMI” or they can say “I have a possible STEMI.” The definite STEMI gets the cath lab alert, the possible STEMI just gives the cath lab a heads up.
If I had such a choice I would have called in a possible STEMI on this one.
I also have to give props to the LP12. After apparently waffling on making a call, it finally came down on the side of the STEMI.
I know there is some talk of having basics in our states get 12-lead monitors that they will not be able to interpret, but if the patient is having clinical signs of an MI and their strip reads Acute MI Suspected, they may be able at some point to activate the cath lab if no paramedic is available on the call.