Every June Rich Kamin, my EMS Medical Director and I give a talk on EMS Stroke Care at our hospital’s annual Emergency Stroke Symposium. This has been going on for a decade now. We are a good team. I am the play by play man and he is the color commentator. I put the presentation together and advance the slides. I may set the scene but whenever we get to the substance, I turn to Rich and say “Doctor…” and he goes into the detailed medical explanation of whatever concept I have raised. We get very good reviews in the evaluations. Then last year, we received this feedback. “They talk about the same stuff every year.”
That hurt. I’m very sensitive.
I mean, yeah, we do talk about the same thing every year . We try to switch the material up some, but it comes back to the same truth.
Time is Brain
EMS is crucial for early stroke recognition and transport/notification to a hospital that can take care of the problem.
EMS Stroke care has changed some over the years; but not as much as in other areas of medicine, and the fundamental truths have never been different.
When I started as a paramedic in Hartford in 1995, our protocol book did not have a protocol for stroke. There was little for us to do prehospitally with a stroke patient, except manage their symptoms. The only real treatment for stroke was thrombolytics that had to be given by the hospital staff within 3 hours of the symptom onset. Paramedics couldn’t give the drug for stroke because before patients can get it they have to have a CT scan to make sure their stroke is an ischemic (caused by a clot) not a hemorrhagic (bleeding) stroke which would rule them out for a drug that busts clots. Giving thrombolytics to a patient already bleeding in the brain could kill them.
Not everyone calls the minute their stroke strikes so we are often arriving past the stroke window or very late in the window. Figuring it takes the hospital an hour to give the drug, we often found ourselves with patients out of the window for the only drug that might help them.
In 2005, the stroke window for us was extended from 3 hours to 4.5 hours from symptom onset for certain patients. That’s the same year we established our first stroke protocol for our region, which basically said do the Cincinnati Stroke Scale (facial droop, slurred speech, weak grip on one side), get a blood glucose to make certain their symptoms aren’t being caused by hypoglycemia (low blood sugar), obtain last known well time (the clock starts not with discovery of the stroke patient, but with the last time they were seen normal), and if you think the patient is having a stroke and is in the 3-4.5 hour window, notify the hospital with a stroke alert so they can start to assemble their team to meet the patient on arrival.
Back then, we actually told EMS not to bring stroke patients to our hospital because we didn’t do a good job of taking care of them in a timely manner. We just weren’t quick enough. Not many hospitals were.
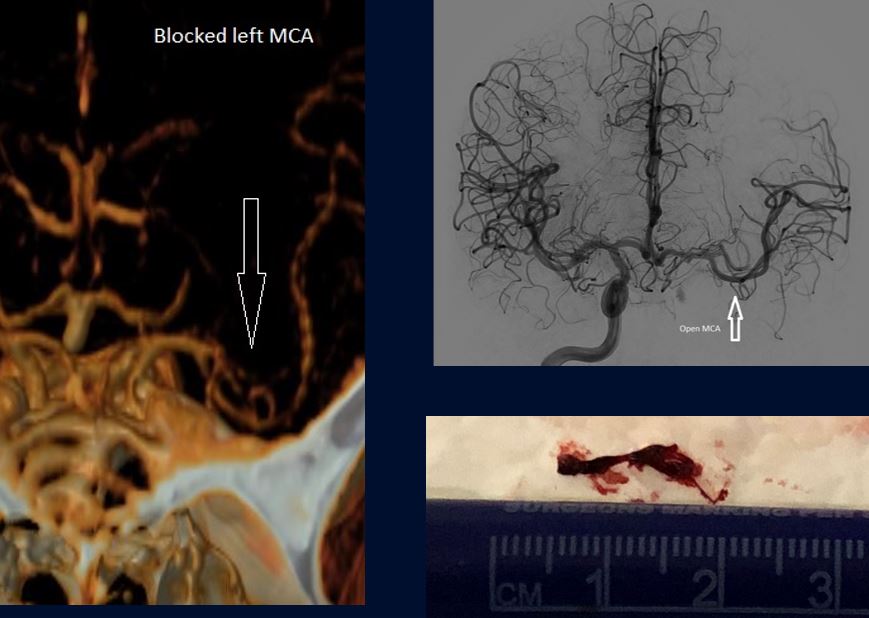
We tried to get better, and succeeded. In 2014, we became an official stroke hospital, which meant we were now meeting rigid standards of care set by the American Heart Association. About the same time we started to host the annual stroke symposium. It wasn’t long before we started doing thrombectomies, a procedure similar to what is done for heart attack patients. Instead of floating a wire into the heart to remove a clock in a blocked coronary artery to restore blood flow, we were floating wires into people’s brains to remove the clot obstructing blood flow –a life-saving procedure.
One of the best things about thrombectomies is they have extended the stroke window out to 24 hours. People out of the thrombolytic window now have hope — at least till the 24 hour thrombectomy window closes.
In 2019, the title of our talk was Stroke Care: Past, Present and Future. That was the first time I read from a book called Once Upon a Time in Connecticut.
“Once upon a time in Connecticut,” I would read, “Would you believe…once upon a time in Connecticut, Traumas were always brought to the closest hospital regardless of capability.”
Many years before back in the 1990s trauma (bad car accidents, shootings, etc,) were always brought to the closest hospital and not to trauma centers. That changed when we recognized getting trauma patients directly to hospitals with the trained surgeons and staff who could save their lives was better than taking them to a hospital that could only for an ambulance to ship them out to a hospital that could better treat their injuries.
“Would you believe that once upon a time in Connecticut, STEMIs were brought to the closest hospital regardless of capability.”
Again, true. It wasn’t until the 2000s that if EMS recognized a patient was having an occlusive myocardial infarction characterized by “ST-elevation” on their ECG that these patients were brought directly to centers that could take then to a cardiac catheterization lab and clear their clots and stent the culprit arteries to restore blood flow.
“Would you believe that once upon a time in Connecticut, Large Vessel Occlusion(LVO) strokes were brought to the closest hospital regardless of capability.”
This was the kicker. They were still brought to the closest hospital rather than a thrombectomy capable hospital and I was saying this really should be changed like we changed the system for trauma and STEMIs.
We were trying to update our regional protocols so that EMS would take patients to a thrombectomy hospital if they were out of the thrombolytic window, but still in the 24 hour thrombectomy window or it they were in the window but within 15 minutes of a thrombectomy hospital.
I have read the same book every year at the stroke conference since then as we have yet to modify our protocol, which still says bring patients to the closest acute stroke ready hospital capable of giving thrombolytics, which is all the hospitals in our region, big and very small.
No change. Why? The small hospitals don’t want to lose not just stroke patients, but all the patients having stroke mimics. And the big hospitals didn’t want to be overwhelmed by all the patients who might be having strokes, but are not. No movement at all. If you are having a LVO and are brought to a hospital that can’t do thrombectomies, you have to get transferred by ambulance to that other hospital. That is very time consuming and time is… you know… BRAIN.
To do something different this year, I decided we would focus again on the Future of Stroke Care. To prepare the talk, I googled “the future of ems stroke care” and found a fascinating article, which I printed out and underlined heavily. It told of a bold future — all the great things that were going to happen in the next decade, including…
Stroke Telemedicine!
CT Scanners in Strokemobiles!
New prehospital medication protocols for stroke to includes neuroprotective, antihypertensive, and thrombolytic therapy!
Only after I had read the article the second time did I notice it had been published in 2013. 12 years ago, and nothing it promised had happened in any significant way.
Sure some big cities have these strokemobiles, but the literature questions their cost effectiveness.
Telemedicine is not a thing in our state, and while it may have a promising future, its effectiveness has not been proven.
And the drug trials — well, they were all busts.
Change in EMS stroke care is slow and sometimes it doesn’t happen at all, but what does not change is that time is brain, and we need EMS to be able to quickly recognize a stroke and get the patient to the right hospital with a prenotification stroke alert.
As far as thrombectomies and triage destination, while it isn’t in protocol, we tell EMS If you are in between a hospital that does thrombectomies and one that doesn’t and you think your patient has a LVO, advocate to take them to the thrombectomy hospital. If your patient is out of the thrombolytic window, but still within 24 hours of their last known well time, take them to a thrombectomy hospital.
Where we once said we wouldn’t bring our spouses to our own hospital if they were having a stroke (we would now) we ask EMS to consider what if their patient were their spouse, where would they want them to go if they were having what they believed was a large vessel occlusion — to a hospital capable of thrombectomy or one not.
Time is Brain.
EMS Decisions Matter.
Still time to register for our free stroke symposium on June 11, 2025. You can attend in person or utilize the virtual option.
Rich and I are speaking at 11:00 AM.

