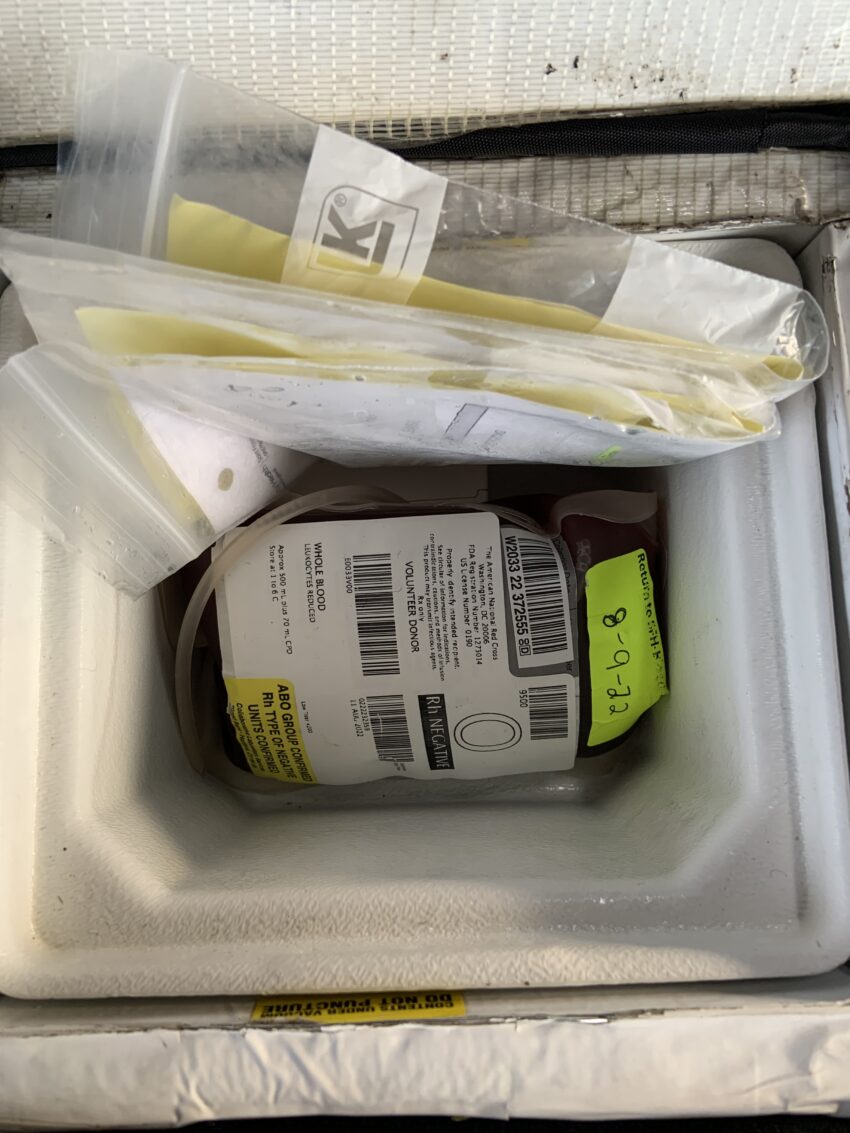
The patient had lost nearly two liters of blood and was barely responsive. I arrived shortly after the primary medic who told me to get the blood set up while he extricated the patient with his partner. As the rapid response medic, I carry the whole blood (0 negative) in a special cooler. I check the temperature at the start of the shift, both by inspecting a temperature sticker on the blood and through an app that uses a temperature stick to monitor the internal temperature of the cooler. I took the 500 cc bag of blood out of the cooler and hung it from a clip on the ambulance wall. I got out the battery, heating cable and special thermal IV drip set. The cable plugs into the battery, then the other end of it plugs into the drip set. I spike the bag just like a bag of saline. It is strange watching blood flow through the line. I am used to flushing a line by letting the saline drip into a trash can or on the ambulance floor. But this blood. I drip it into a trash can. Once activated the coil in the line heats the blood to body temperature. It takes about thirty seconds. The lights on the cable flash from blue ( not ready) to green (all set to go), By the time I had the bag spiked, the crew was sliding the patient on the stretcher next to me. Her veins were flat and hard to find. She had no radial pulse. I got an IV on my second try and then hooked the blood to the end of the lock. We attached a pressure bag to the blood to speed its delivery, and then were on our way, calling in a trauma alert. In the five minutes we transported, the patient went from no radial pulse to a strong pulse and she was no longer so ghostly white.
There are medications that we carry in EMS that are miracle drugs where we see the results in front of our eyes. Epinephrine for anaphylaxis. Narcan for opioid overdoses. Dextrose for hypoglycemia. Adenosine for SVT. Benzos for seizures. I would add, at least in this case, whole blood for hypovolemic shock.