You are dispatched to the zoo for a snake bite. There you find the reptile keeper in extremis. He says he has been bitten by a deadly mamba snake and if he is not soon administered the antivenom, he will die. You don’t carry antivenom in your med box, but there is antivenom there at the zoo. To administer the antivenom, you have to start an IV, which you are allowed to do, then you mix the antivenom up and run it in a drip. But antivenom is not a med in your formulary and you don’t know anything about it other than this guy is telling you he is going to die unless you give it to him. You are not certain so you call your medical director, but you are unable to make contact.
What do you do?
This is a situation EMS responders found themselves in (at least according to news reports) in Kentucky.
What did they do? They gave him the antivenom. He still spent days in the ICU, but he lived to tell about it. His wife and many physicians say they saved his life.
Now the medics for their good deed have to go before the Kentucky EMS board to explain their actions.
They have said even if they lose their licenses, they would do it again. They say they had a moral and ethical responsibility to save the man’s life even if it went against rules.
The hearing is scheduled for tomorrow. What will happen there? Will the board tear up their licenses or will they give them a slap on the wrist and then hero’s medals?
There are perhaps details and circumstances to this call that I am not aware of, so we can keep it hypothetical.
What would I do in their situation?
A good friend of mine and EMS Medical Director likes to say, “It depends.” You can’t have a protocol for every situation and medics are supposed to use their best judgement within the context of their training and scope of practice. Your actions depend on many factors.
For me, if I had been there, I would certainly put a lot of stock in the fact that the snake handler reptile expert is telling me he will die unless I give him the antivenom. He is so knowledgeable about antivenom that he has a stock of it right there just in case he gets bitten. If a lay person was telling me he would die unless I gave him antivenom, I might act differently. But I give great deference to the opinion of this reptile expert.
Here in Connecticut while we do not yet have a snake bite protocol, we do have two protocols that might apply in this situation.
1.2 Exception Protocol
We recognize, though, that on rare occasion, good medical practice and the needs of patient care may require actions not otherwise authorized by these protocols, as no protocol can anticipate every clinical situation. In those circumstances, under this Exception Principle, EMS personnel are authorized to take actions not otherwise explicitly authorized under these protocols provided that:
1. Such action is within their current EMS certification, licensure level, and scope of practice,
AND
2. They have obtained the approval of direct medical oversight.
So in this case:
- Doing an IV and administering medication through an IV is within the paramedic’s scope of practice.
- Since they were unable to make contact with direct medical oversight, see Communications Failure Protocol
6.4 Communications Failure
In case of a communications failure with Direct Medical Oversight due to equipment malfunction or incident location, the following will apply:
EMS personnel may, within the limits of their certifications, perform necessary ALS procedures that under normal circumstances would require a direct physician order. These procedures shall be the minimum necessary to prevent the loss of life or the critical deterioration of a patient’s condition. All procedures performed under this order, and the conditions that created the communications failure, need to be thoroughly documented.
In Connecticut, the EMS providers would have to do the following:
The EMS provider shall provide a written notification pertaining to the action taken describing the events including the patient’s condition and treatment given, and referencing the EMS Incident Report. This report must be filed with the Sponsor Hospital’s EMS Medical Director, Hospital EMS Coordinator, and Office of EMS within 48 hours of the event.
Hoping for a just outcome for these EMS clinicians.
*****
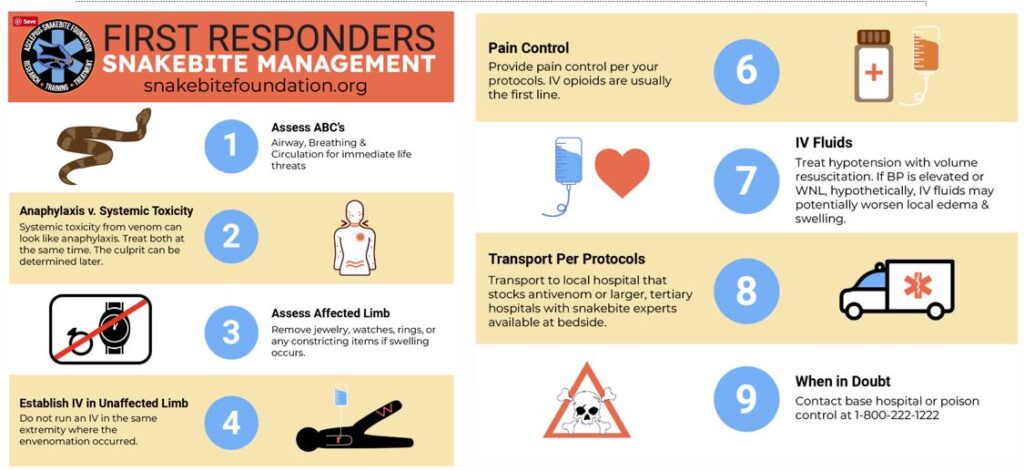
How to Treat Snakebites for First Responders in the United States